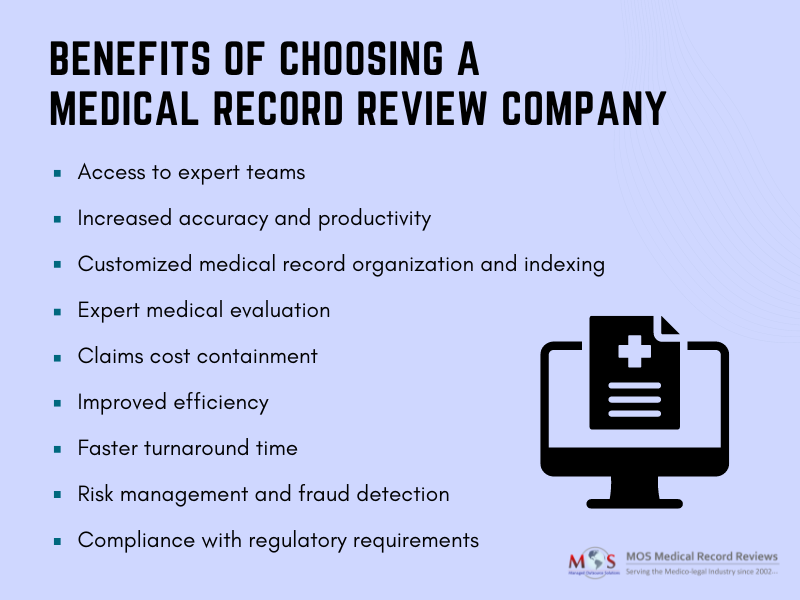
In the insurance industry, ensuring accurate and fair claims processing is crucial for both insurers and policyholders. To speed up claims processing and reduce the complexity involved, insurers, insurance attorneys, law firms, and adjusters utilize medical review services provided by experienced medical review firms. Experienced companies providing medical record review for insurance companies assess the validity and appropriateness of medical claims. Such companies employ experienced and qualified healthcare professionals who possess in-depth knowledge of medical procedures, treatments, and best practices. These experts review medical records and related documentation to assess the necessity and appropriateness of the services rendered. Their expertise ensures accurate and unbiased evaluation, reducing the risk of erroneous claim approvals or denials. Insurers can rely on the medical review service’s expertise to make informed decisions and minimize potential disputes.
Partnering with a trusted medical record review company helps insurers contain claims costs effectively. Medical review services play a vital role in reducing fraudulent or abusive billing practices, contributing to overall claims cost containment. By conducting comprehensive reviews of medical records, treatment plans, and billing codes, these services can identify unnecessary or excessive treatments, procedures, or billing errors. Insurers can then make informed decisions regarding the coverage and reimbursement of such claims, resulting in cost savings and improved profitability.
Partner with us for better insurance operations!
Save time and resources with our comprehensive medical record review services.