Achieving optimal performance in the Healthcare Effectiveness Data and Information Set (HEDIS) quality measures is pivotal for payers aiming to provide high-quality care and promote better health outcomes. Healthcare plans need HEDIS medical record reviews to gauge their performance across vital dimensions of care and service quality. Payers engage in HEDIS assessments to enhance the quality measurements of their Medicare Advantage plans, commonly referred to as Star Ratings. These ratings were established by the Centers for Medicare & Medicaid Services (CMS) to evaluate the performance of health plans within Medicare Advantage programs and Medicare risk adjustment initiatives. The HEDIS review metrics constitute a segment of the comprehensive Star Ratings system. A payer’s overall rating is contingent not only upon medical record review outcomes but also customer satisfaction, pharmacy metrics, and operational efficiency.
The data gleaned from medical record reviews is sent to third-party vendors responsible for collating and submitting the information to the National Committee for Quality Assurance (NCQA) by the month of May. The NCQA then assesses and publishes the annual Star Ratings. These ratings are also released annually on the CMS website, ensuring that patients and the broader healthcare sector remain informed about the performance levels of diverse healthcare plans.
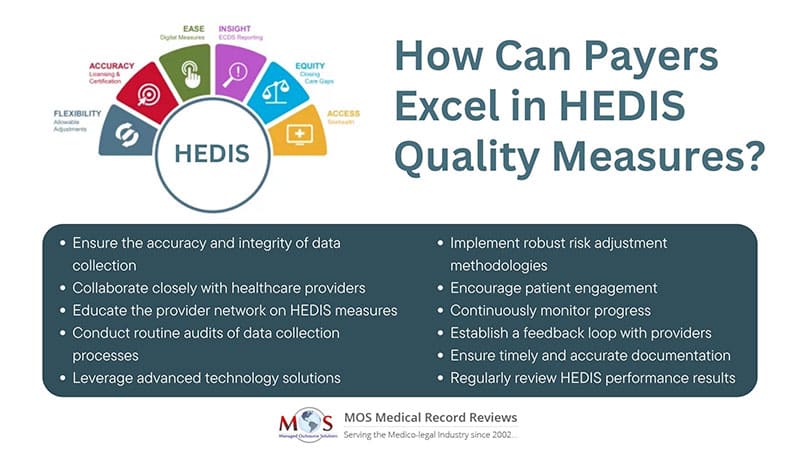
How to Improve HEDIS Quality Measure Performance?
Here are some valuable tips to help payers improve their HEDIS quality measure performance:
- Data accuracy and integrity: Ensure the accuracy and integrity of your data collection processes. Implement robust data validation and cleansing procedures to prevent errors and inconsistencies.
- Provider collaboration: Collaborate closely with healthcare providers to enhance care coordination and information sharing. Clear communication and collaboration can help with more accurate documentation and reporting.
- Education and training: Educate your provider network on the importance of HEDIS measures and the specific documentation requirements. Offer training sessions to help providers accurately report data.
- Regular audits: Conduct routine audits of your data collection processes to identify and rectify any discrepancies or issues. This proactive approach can help maintain data accuracy throughout the reporting period.
- Technology utilization: Leverage technology solutions such as electronic health record (EHR) systems to streamline data collection and reporting. Automation can reduce manual errors and improve efficiency.
- Risk adjustment: Implement robust risk adjustment methodologies to account for variations in patient populations and ensure fair comparisons among different plans.
- Patient engagement: Encourage patient engagement and participation in preventive care and screenings. Effective communication can help ensure improved compliance with recommended care measures.
- Performance benchmarks: Establish performance benchmarks based on historical data and industry standards. Continuously monitor progress and compare against these benchmarks to identify areas for improvement.
- Continuous improvement: Maintain a culture of continuous improvement. Regularly analyze performance data, identify trends, and implement targeted interventions to address gaps.
- Feedback loop: Establish a feedback loop with providers to share HEDIS performance data. This transparency can foster accountability and motivate providers to improve their care delivery.
- Timely documentation: Ensure timely and accurate documentation of patient care activities. Encourage providers to document care promptly to prevent missing out on reporting opportunities.
By implementing these strategies, payers can proactively enhance their HEDIS quality measure performance, leading to better care outcomes, improved member satisfaction, and strengthened relationships with healthcare providers.
Request a comprehensive medical record review!




