Medical record analysis is an important step in claims processing and helps determine patient eligibility for a particular procedure or treatment. When the traditional model of medical record review can be laborious and time-intensive, review processes done using advanced AI are very efficient and accurate, apart from being much quicker too. In AI-powered document review, machine learning algorithms are used to automate the processes of reading, reviewing and categorizing the medical records; the volume of records is not a concern at all. This technology accurately and quickly identifies patterns, categorizes the documents, and highlights important details.
AI-powered medical chart review can identify relevant medical evidence up to 60% faster than a purely manual review. Providers utilize the latest machine learning and language models with medical and legal Deep Learning to ensure accuracy.
AI Use in Medical Claims Review
Once the paperwork associated with medical claims review is avoided, the insurance industry get to benefit from smoother and more accurate document review. In complex claims, even minor details are very important and have an impact on the outcome of the claim or case. Moreover, when document sorting and indexing are automated, the time saved can be used more productively. The claims can be reviewed more thoroughly and in lesser time. Apart from time and cost savings, AI use in claims processing can also improve customer satisfaction.
Get a free consultation today and see how MOS Medical Record Reviews can provide a customized solution for your specific needs.
AI tools are powerful and can quickly scan and understand the content of medical records. They can identify significant information, and easily detect any inconsistencies or ambiguities in the charts. Here are some of the types of insurance-related medical documents that AI tools can successfully review.
- Statements from attending physicians
- Electronic medical records
- Claim forms
- Prescription data
- Pharmacy records
- Lab results
- Imaging records
- Insurance applications
- Medical billing data
- Handwritten notes
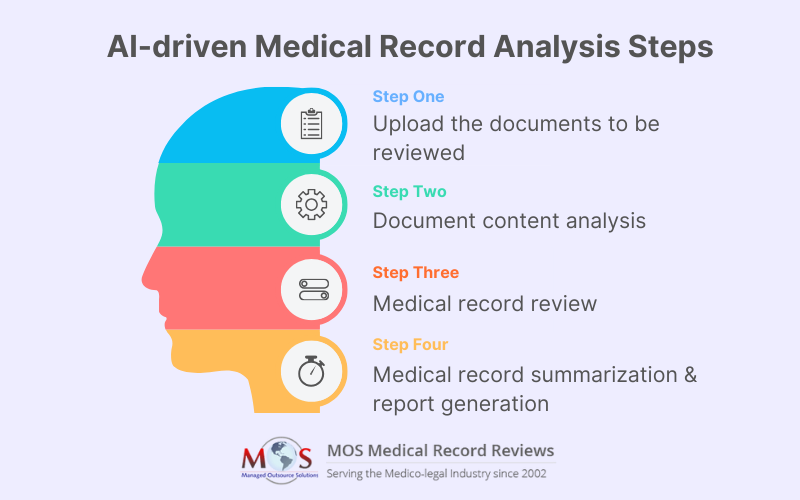
The Medical Record Review Process Using AI Tools
- Upload the documents to be reviewed: The document upload can be done in bulk into the AI system. The platform starts to work with its automated workflows.
- Analysis of the document content: The AI system uses machine learning and natural language processing to review the content. Important information is extracted and categorized properly.
- Medical record review: The review is done comprehensively focusing on your particular needs. The AI system flags potential issues, inconsistencies, anomalies and so on for human review. This additional human review ensures accuracy and also enables any adjustments necessary.
- Medical record summarization and output generation: The system generates an insightful report or summary of the findings. The key findings are highlighted. This makes it easy to review the important points and take necessary actions.
Advantages of Using AI Tools for Medical Claims Review
Let us look at the various tangible advantages of using artificial intelligence solutions for medical document analysis for insurance claims processing.
- You can file the claims more quickly, ensuring maximum accuracy.
- AI tools help with fraud detection. Historical claims data can be analyzed to identify suspicious patterns or inconsistencies that indicate fraudulent activities. This will help insurers to distinguish between legitimate and fraudulent claims and deny the latter. Machine learning models can be trained to understand and adapt to various fraud tactics including evolving ones, which helps improve detection accuracy over time.
- The entire claims review and processing workflows can be streamlined. The AI algorithms verify the completeness and accuracy of claims, thereby reducing manual errors and speeding up the overall process.
- AI tools provide predictive analytics that is very important for insurers. The insights made available enable payers to assess risk, make informed decisions, prioritize claim reviews and distribute resources effectively. As a result, they benefit from enhanced financial outcomes and improved service delivery, and ultimately better customer satisfaction.
Artificial intelligence algorithms that can read, understand and sort data, and channelize the relevant information to human reviewers for specialized analysis are all set to change the insurance and claims processing landscape. As service providers point out, you can expect around 70% faster claims processing, more accurate results, and smoother workflows. There is no doubt whatsoever that AI systems will continue to be used more effectively in the medical and insurance industry with the best possible results. When choosing a service provider, it is vital to make sure that they are committed to ethical and responsible use of AI, and are compliant and transparent in their dealings.
Benefit from accurate, faster, and more efficient claims processing with MOS’ AI-powered medical record review.