Medical peer reviews are crucial for clean health insurance coverage. In case of a doubt or ambiguity regarding a medical insurance claim, a medical peer review may be conducted by a physician employed by the insurer. Conducting such a review helps to decide whether the medical services provided by the treating physician were medically necessary. A negative review or comment on the part of the peer review physician could lead to claim denial.
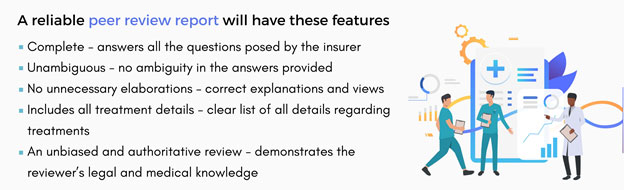
For good peer review reports, insurers can consider partnering with an experienced medical review company. Such companies provide the services of skilled reviewers knowledgeable in the contractual language of the plan and the various medical aspects involved. A clearly written peer review report serves as a helpful legal document for claim denial or acceptance and clarifies everything for the claimant, the physician, and the attorney.